The problem
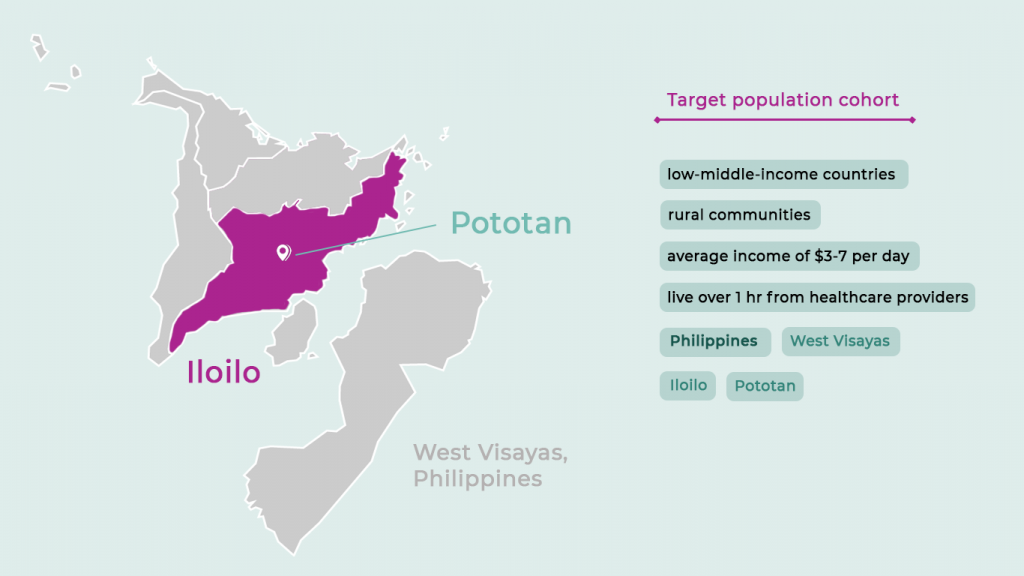
79% of people living with diabetes are in low-and-middle income countries – a disease that kills 4.3 million people per year. The majority are unable to access the affordable medicines, diagnostics and education they need. 4 in 5 people with diabetes in low-and-middle income countries are undiagnosed.
In these rural populations, there is a lack of education and diagnosis of diabetes and hypertension. As a resident in the areas, you typically have to travel long distances to expensive private clinics for basic tests for glucose, HbA1C and cholesterol. A comprehensive panel costs approximately $50 in a private hospital or outpatient diagnostic centre, 10 times more than the average daily earning of a community resident.
There are also shortages of health workers in Pototan, with a doctor to population ration of 1:78 298 compared with the WHO benchmark of 1:1000
Campaign objectives
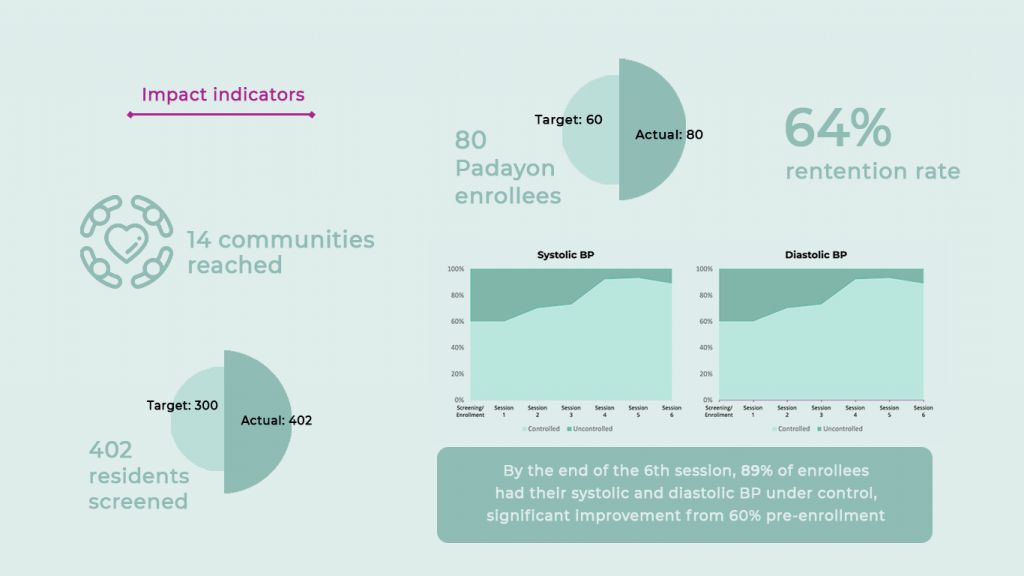
- To evaluate the effectiveness and scalability of the ‘offline-first’ digital health intervention in managing diabetes and hypertension in low-resource setting
- To assess the impact of the intervention on patient outcomes for diabetes and hypertension
- change in systolic/diastolic blood pressure (BP).
- change in RBS.
- change in knowledge of diet and nutrition.
- change in understanding of diabetes and hypertension complications.
- member retention rate.
- Overall lives improved (definition: patients able to put their previously uncontrolled systolic/diastolic BP numbers and/or RBS numbers into target range in at least one point during the programme).
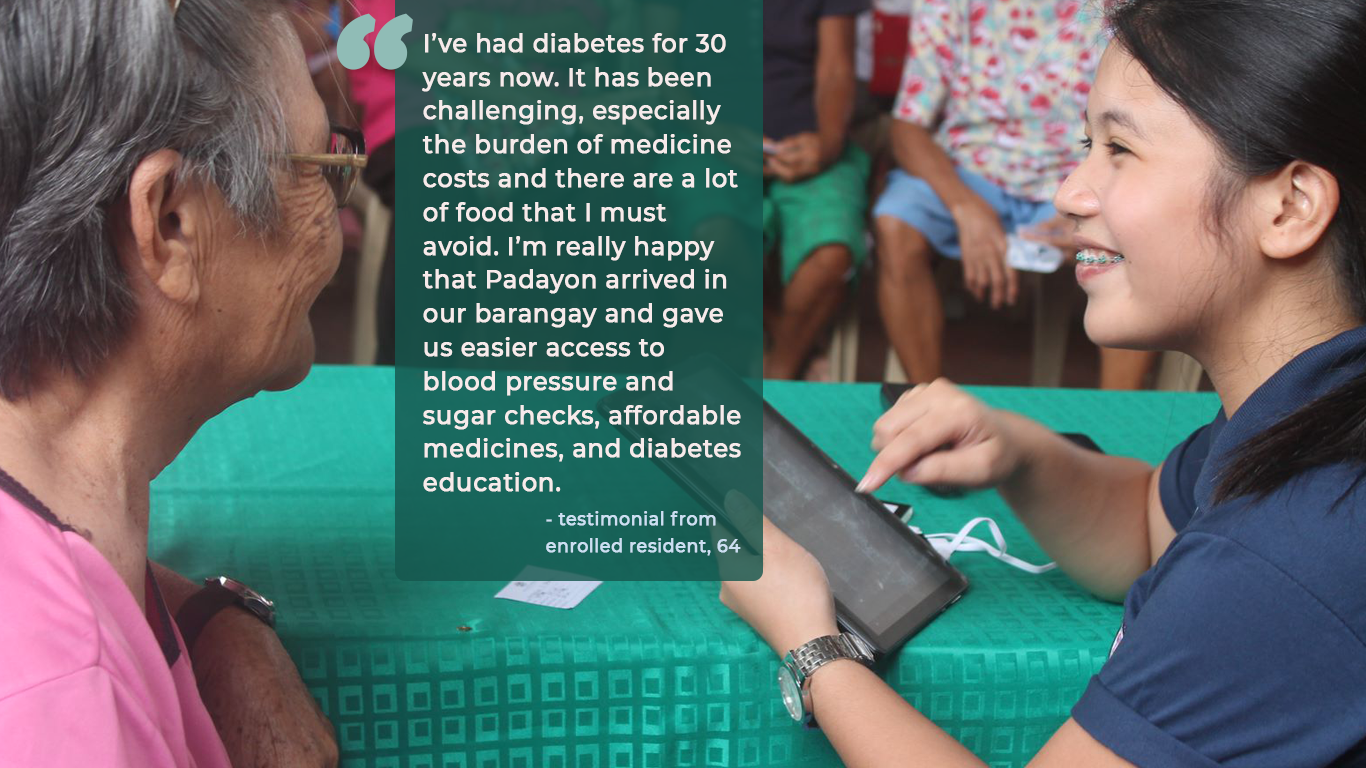
This campaign spotlights ‘Padayon’ (meaning keep moving forward) – a new digital health model that demonstrates the benefits of task-shifting from traditional skilled health workers to community health teams with the help of reach52 access, our offline-first app that supports a fully integrated solution for low-income patients providing coaching, testing and medicines in one accessible subscription service.
This new model of care to transform diabetes and hypertension outcomes for rural populations focuses on
- a holistic patient solution for education, testing and medicines
- Community-based model of care, bringing support closer to patients
- a repeatable and scalable model that can be implemented across LMICs
Holistic subscription service
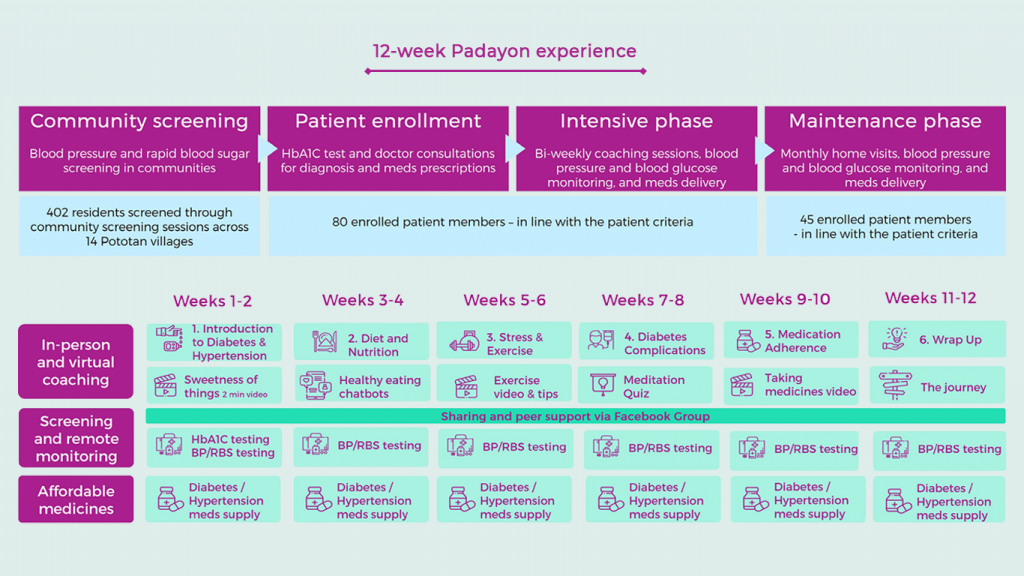
For 996 PHP ($20), residents receive a 12-week subscription programme covering:
- Quality, discounted Diabetes or HT medicines delivered directly to them (via reach52 marketplace)
- BP and random blood sugar glucose checked bi-weekly & entered into app for remote monitoring
- 12-Week Coaching Program with their own trained Health Coach
- 6 face-to-face coaching sessions (Nutrition, Exercise, Stress Management, Medication Adherence, Disease Complications, Problem Solving)
- Supported by guided tasks in between F2F sessions and virtual learning – bite-sized videos, ‘how to’ checklists and FB peer group
- Certificate and recognition for completing the 12-week programme
- All these at a subsidised rate (less than half of actual cost to patients) to enable patient-pay model
Insights
- Training members of communities as Agents and equipping them with ‘offline-first’ platforms and mobile health apps can overcome traditional access barriers for non-communicable diseases (NCDs) in low-income and middle-income countries.
- Integrating coaching, screening and medicines into a simple subscription service delivered by ‘digitised’ community members has the potential to significantly improve health outcomes in low-connectivity, low-resource settings
- There is patient willingness to pay for digital subscription services for diabetes and hypertension even in populations on an average income of $3-7 per day
- Quality health data can be collected through community Agents trained to use our offline-first reach52 access app, enabling remote patient monitoring and analysis for population-level precision healthcare